The month of March marked the 4th year anniversary of the Covid pandemic as it hit the United States. Who can forget when Vice President Mike Pence announced the White House’s “15 days to slow the spread” campaign? It was an unprecedented initiative by the federal government to begin lockdowns, school closings, and other sweeping measures to mitigate the spread of Covid-19, a novel coronavirus that came to us from China.
Four years later we can assess the damage done by those measures and evaluate their effectiveness in containing the virus. Unfortunately, the analysis is ugly. Dr. Scott Atlas, Stanford University Medical School professor, and Steve H. Henke, professor of applied economics at Johns Hopkins University, tell us the sordid truth in an article published in The Wall Street Journal. They say, “None of those policies were successful, and many were gravely damaging.”
They tell us the Covid health benefits of mandatory lockdowns were tiny. Lockdowns in the U.S. prevented between 4,000 and 16,000 Covid deaths. In an average year 37,000 Americans die from the flu, according to the Centers for Disease Control and Prevention. Lockdowns also failed to reduce infections more than a trivial amount, in part because people voluntarily alter their behavior when a bad bug is in the air. Coercive government policies generated few benefits—and massive costs.
Public-health agencies exacerbated the damage by failing to keep their heads and follow standard pandemic-management protocols. Before 2020, it was recognized that communities respond best to pandemics when government measures are only minimally disruptive. During Covid, however, officials junked that practice by green-lighting restrictive practices and intentionally stoking fear. That response overlaid enormous economic, social, educational and health harms on top of those caused by the virus.
Those harms are captured, in part, in excess deaths—the number beyond what would have been expected without a pandemic. Non-Covid excess deaths from lockdowns, the shutdown of non-Covid medical care, and societal panic are estimated at nearly 100,000 between April 2020 and at least the end of 2021. The number of lockdown and societal-disruption deaths since 2020 is likely around 400,000, as much as 100 times the number of Covid deaths the lockdowns prevented.
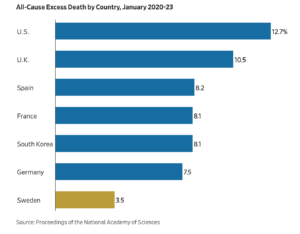
The best measure of health performance during the pandemic is all-cause excess mortality, which captures the overall number of deaths relative to the expected level, encompassing Covid and lockdown-related deaths. On this measure Sweden—which kept most schools open and avoided strict lockdown orders—outperformed nearly every country in the world.
A recent study published in the Proceedings of the National Academy of Sciences found that the U.S. “would have had 1.60 million fewer deaths if it had the performance of Sweden, 1.07 million fewer deaths if it had the performance of Finland, and 0.91 million fewer deaths if it had the performance of France.” In America, states that imposed prolonged lockdowns had no better health outcomes when measured by all-cause excess mortality than those that stayed open. While no quantifiable relationship between lockdown severity and a reduction in Covid health harms has been found, states with severe lockdowns suffered significantly worse economic outcomes.
What was the impact of closing hospitals and cutting off access to non-Covid healthcare?
The authors tell us, “Closing hospitals and cutting off access to non-Covid healthcare generated a fear of entering medical facilities. That was a profound mistake, as was encouraging the false belief that hospitals were too busy to treat people who needed care. Healthcare utilization rates were at low levels between 2020 and 2022. In spring 2020, nearly half of the nation’s some 650,000 chemotherapy patients didn’t get treatment, and 85% of living organ transplants weren’t completed. One study found that there were 35.6% fewer calls for cardiac emergencies after March 10, 2020, compared with the year prior. Emergency-room visits were down between 40% and 50%, according to an estimate in May 2020. That doubtless contributed to observed non-Covid excess deaths and may continue to do so, as Americans suffer from undetected cancers and other long-term conditions. Healthcare uptake is still lower than pre-pandemic levels.”
While school closings had no offsetting public-health benefits, the attendant isolation led to massive increases in psychiatric illness, self-harm, obesity and substance abuse. Healthy children were always at vanishingly small risk from Covid, and nearly all of them were infected at some point anyway, according to CDC data. Like a regressive tax, these harms were severest for lower-income and minority students.
Unfortunately, this experience has left many Americans wondering where to turn for honest, accurate information in a medical crisis. They have lost faith in our public-health institutions. It’s not clear how that faith can ever be restored.

